Statistics relating to the incidence of TMJ Disorders (TMJD) and Sleep Apnea are often quoted around 70%.
In my specialty practice, I see above 50% of people presenting with TMJ problems also have undiagnosed sleep-breathing problems (Sleep Apnea, UARS, Fatigue).

One of the many reasons these conditions are linked is the fact that an obstruction of the airway during sleep often triggers an episode of clenching or grinding in an effort to stiffen (open) the airway. This is done while asleep, so it is usually discovered at a dental appointment when you are told your teeth “look like you have been clenching or grinding”.
Long term clenching and grinding slowly damages the TMJ cartilage disc and triggers arthritis in the TMJ. Dental nightguards do not stop clenching or grinding, nor do they necessarily protect the TMJ joint. They are designed to protect the teeth only.
An article this week describes link between Rheumatoid Arthritis (of the TMJ) and Sleep Apnea. Those of us who treat TMJD intuitively know this and it’s encouraging when research appears that supports our clinical observations.
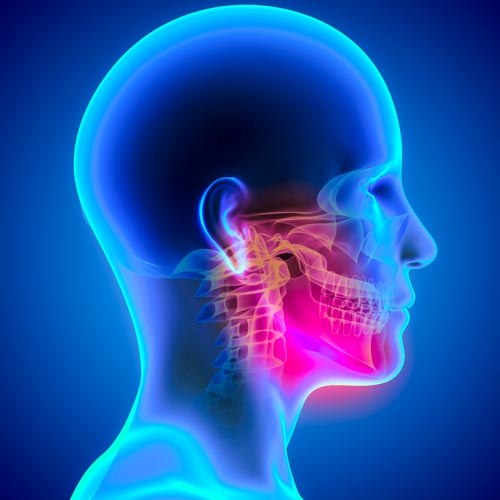
When the TMJ (jaw joint) has either a disc that dislocates (any clicking in the TMJ means the cartilage has been torn off the bone) or develops the arthritis that follows disc displacement – it causes the entire jaw to move slightly up and back. This is because the jaw joints lose their support and stability. As the lower jaw slides backwards, it sometimes shows up as a change in your bite (occlusion). Often feeling like a back tooth or teeth are sore, hit harder than the rest of the teeth, or your front teeth no longer fit together when trying to bite into something.
Rheumatoid arthritis is a genetic condition where the body attacks and destroys cartilage and bone in various joints. The pain caused can disturb sleep, often triggering clenching. If the TMJ joint is involved, it causes the jaw to slowly collapse backwards over time. The support of the airway is decreased as the muscles under the chin fall back, often narrowing the airway during sleep.
The article also relates arthritis in the upper neck to have an effect on the size of the airway, contributing to a loss of airway support at night.
If you find your sleep becoming less refreshing, if you are told that you are grinding/clenching your teeth, have neck pain or popping/noise in the jaw joints, it should be evaluated by a Dentist specializing in TMJ and Sleep Breathing Disorders. I work with a network of medical professionals to help evaluate complex conditions and get to the source of problems.
The Link Between Sleep Apnea and Rheumatoid Arthritis